Why You Shouldn't Drive after Pupil Dilation
Alzheimer’s disease is probably one of the most terrifying prospects any of us can consider. It is a disease that robs us of our minds, casting aside coherent thought, memory, and likely any sense of identity. Recently, several groups have identified interesting ocular associations with Alzheimer’s disease, enabled by our unique ability to directly visualize intraocular tissue. I am asked about these associations every now and then by savvy patients, and I thought it would be interesting to share what I have learned for this month’s article.
Background
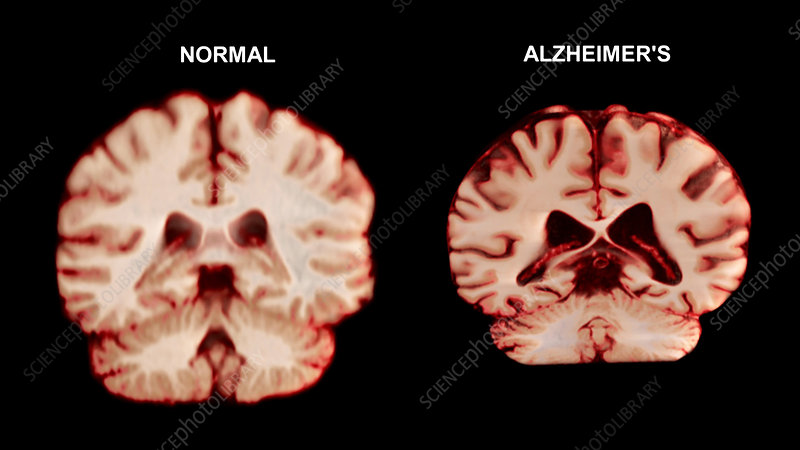
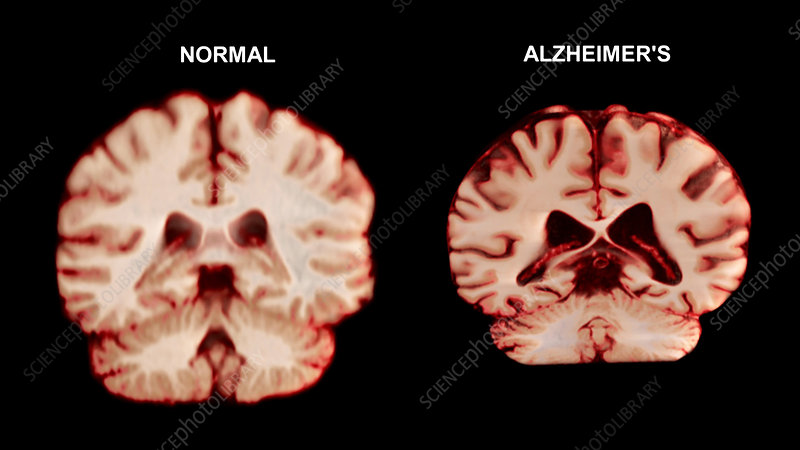
Alzheimer’s disease is a type of dementia that affects memory, thinking, and behavior. It is the most common form of dementia, accounting for 60-80% of all cases. Changes in the brain generally begin at least a decade before symptoms manifest. Abnormal deposits of beta- amyloid plaques and neurofibrillary tau tangles throughout the brain lead to abnormal brain function. Over time, neurons lose the ability to communicate and eventually die.
Ocular Findings
Several smart physician researchers have noted interesting anatomic ocular findings associated with Alzheimer’s disease. Gharbiya nd associated found thinner choroidal thickness on enhanced depth imaging OCT in patients with Alzheimer’s disease compared to age- matched controls. Variations of choroidal thickness is seen in other diseases as well, including thinning of the choroid in eyes with macular degeneration, glaucoma, diabetic retinopathy, and retinitis pigmentosa. We also see a thinning of the choroid after a course of anti-VEGF treatment for macular degeneration. On the other hand, choroidal thickening is a classic finding in central serous retinopathy and Vogt-Koyanagi Harada disease. Another interesting finding is lower levels of macular pigment in patients with Alzheimer’s disease. Both of these findings, however, are rather nonspecific and of minimal clinical utility.
Perhaps the most interesting recent developments are two imaging modalities that appear to be able to detect beta amyloid plaques in the retina. Neurovision Imaging out of Sacramento uses retinal image fluorescence photography to look for a characteristic fluorescent signature of the plaques. Prior to the imaging study, patients take curcumin, the ingredient in turmeric that gives it its yellow color. Data on 40 subjects showed that levels of the amyloid in the retina correlated closely with levels of amyloid in the brain on PET scan (100% sensitivity and 81% specificity). This imaging technique might be available as early as the 2nd half of 2015.
A second company, Cognoptix out of Massachusetts, has developed a similar imaging technique, the SAPPHIRE II. Their technique uses fluorescent ligand eye scanning (FLES) process in which a topical ointment is applied to the eye. The scanner can then detect beta-amyloid plaques. Data from 40 patients showed 85% sensitivity and 95% specificity.
I will be very interested to see the public’s reaction once these tests are available. Will people be lining up at the doors of doctors who purchase a machine, where they would probably serve little good, or will these be exclusive to research institutions where they may serve as non-invasive ways to monitor disease progression and response to potential therapies? With no real prophylactic therapies will people want to know if they might develop Alzheimer’s disease in the next few decades? I’m not sure I would. Would you?
Thanks again for reading. Please don’t hesitate to contact me with any questions.
Schedule a Retinal Consultation in San Diego
If you would like to refer a patient experiencing a retina-related issue, we encourage you to contact Retina Consultants San Diego.