A Note From Our Team
Vitreous and Retinal disease can be confusing to anyone not trained in the field. It’s easy to forget this in a busy clinic. However, we believe that it is critical for you as a patient to understand as much as possible about your condition, the anatomy involved, how we evaluate your eye, how your condition might progress, and the treatment options. Below is a brief overview of the anatomy of the eye, our imaging and diagnostic instruments, as well as a short description of several of the more common conditions we treat. We hope that you find this helpful and that it facilitates your understanding, but if you have any questions please ask. Furthermore, we encourage anyone suffering from insomnia to read this immediately before going to sleep.
- The Physicians of RCSD
Anatomy of the Eye
Think of the eye like a camera. Light comes in through the front, first passing through the cornea, through the pupil which is the black circle surrounded by the colored iris, through the lens, which develops a cataract as we age, through the large vitreous cavity where floaters may develop, and eventually hitting the retina. Like a camera, the lens and cornea help to focus light onto the retina to produce a clear image. Similar to film, the retina collects the image and sends it to the brain via the optic nerve for interpretation.
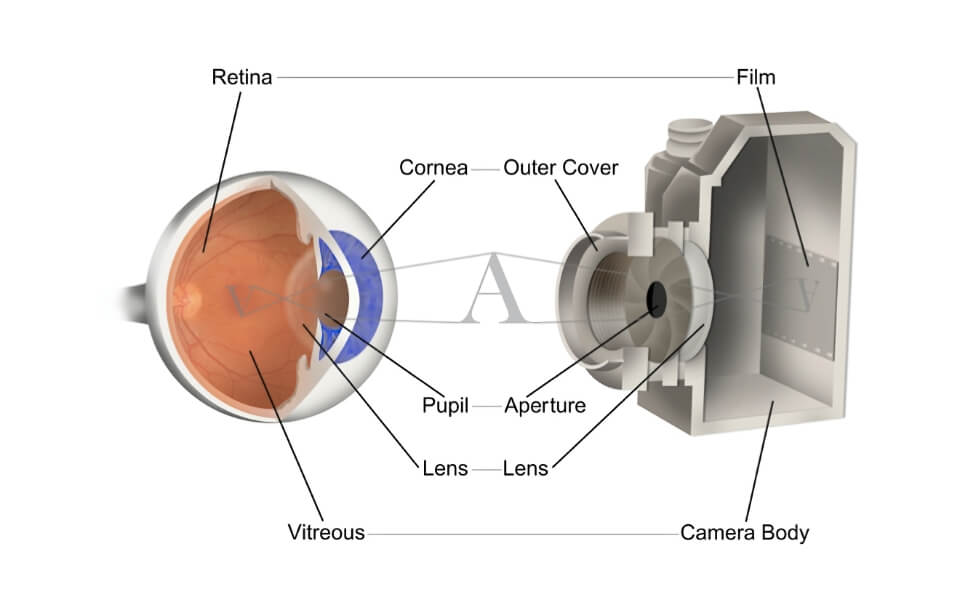
Figure 2 shows a cross section of the eye. The retina is very thin, delicate, and lines the back wall of the eye like wallpaper on a wall. Blood vessels visible in the retina supply oxygen to the inner half of the retina. Beneath the retina is an important tissue layer called the retinal pigment epithelium. Beneath this is the choroid - a dense layer of blood vessels that supplies oxygen to the outer half of the retina.
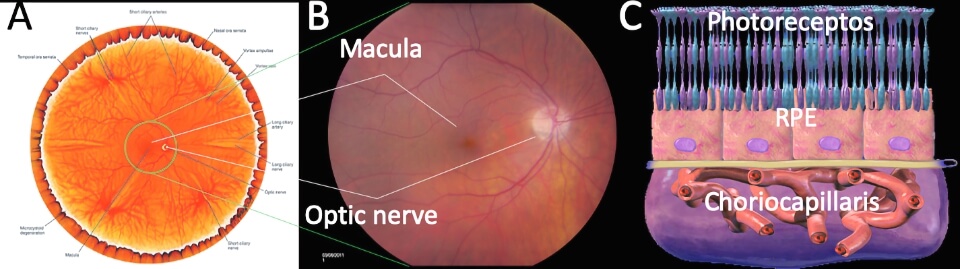
The middle picture shows a color photograph of the central 50 degrees of a right retina. You can see the circular optic nerve on the right side. The optic nerve is a bundle of nerve processes from all of the photoreceptors (rods and cones), arranged in the wall of the nerve like a pipe. The center of the optic nerve has blood vessels entering and exiting the eye. These blood vessels fan out into the retina, supplying the inner half of the retina with oxygen. In the photo these are the red lines; you can see the large vessels leaving the optic nerve and wrapping around the middle of the retina to the left. The area of the retina surrounded by these vessels is called the macula with the fovea being the brown spot in the very center. The macula is the center of the retina, like a bullseye is the center of a dartboard. It has a high density of photoreceptors, and is very important for clear vision.
While the back wall is lined by the retina, there are several important layers of tissue beneath this. The third picture shows a schematic of what the back wall of the eye looks like in cross section with retinal photoreceptors at the top, a single layer of cells beneath this called the retinal pigment epithelium, and a layer of blood vessels called the choroid. The RPE performs all of the custodial functions for the retina, and without it the retina cannot survive. The choroid is very high in blood flow, and provides oxygen to the outer half of the retina. Each of these three layers can play an important role in retinal disease.
During your visit we will obtain several diagnostic studies, in addition to an examination. These commonly include color photographs of your eyes, optical coherence tomography, and fluorescein angiography (figure 3).
![Optical coherence tomography [OCT] scans and fluorescein angiography photos of the retina.](https://www.rcsd.com/media/pages/services/retina-101/c38c1bdbed-1617644046/rcsd-figures.003.jpeg)
Optical coherence tomography is similar to an ultrasound that uses light instead of sound waves. The light is reflected off the back wall of the eye and the reflectance of the different tissues is measured (eg. clear liquid does not reflect and appears black, dense tissue such as the RPE reflects a lot of light and appears bright). In a normal retina (figure Xc) the retina appears as a striped gray structure flat on the RPE, which appears as a bright white band. The retina has a small dip at the fovea. The choroid is visible beneath the RPE with a honeycomb pattern and the optic nerve is visible exiting the back of the eye.
Fluorescein angiography allows us to evaluate your retinal and choroidal blood vessels, and to look for areas of leakage or inflammation.
In addition to the above, other studies may be ordered on a case-by-case basis, including ultrasound, macular microperimetry, dark adaptation, indocyanine green angiography, and fundus autofluorescence.
Among the unique features of our practice, RCSD offers sophisticated dark adaptation and macular microperimetry testing of macular disorders.
Dark adaptation is a simple but sensitive test that assists with the diagnosis of drug toxicities, nutritional deficiencies, inherited retinal dystrophies and age-related macular degeneration. This relatively easy test measures the speed at which an eye adapts to darkness after exposure to a bright flash of light. It may be offered to patients who complain that they cannot see in the dark and have trouble adjusting to a movie theatre or other dark room after walking in from a brightly lit environment. The results of this test provide valuable information about the function of the retina and the chemistry of vision. Dark adaptation testing can determine whether there is a fundamental problem with the ability of an eye to adapt to darkness or whether the symptoms are simply normal for a specific age range. The results of this test have been used to identify vitamin A or zinc deficiencies, diagnose chloroquine, plaquenil, elmiron or other drug toxicities and study the fundamental cause of outer retinal dystrophies or degenerations. To perform the test, the patient is comfortably positioned and asked to focus on a small red target in a large dome. A brief flash of light is delivered just below the central vision and the patient is asked to press a button when they see a green circle within the after image of the flash. Over a period of time, the green circle fades to a fainter green circle and eventually turns into a white circle that eventually becomes dimmer. The test ends when the eye is capable of seeing a specific intensity of dim light. The results of the test are reviewed with the patient and the referring physician.
Macular microperimetry is another simple but highly sensitive test that is often used to reassure patients that there is no evidence of side effects from drugs that are used to treat medical disorders. Macular microperimetry also assists with the diagnosis of drug toxicities, strokes, glaucoma or macular scars and blind spots located close to or directly in the central vision. This test measures the sensitivity of an eye to ambient light and can pick up small defects that may be missed on routine exams. A unique feature of this test is that the central visual field can be superimposed over a color photograph of the macula which allows the structure of the macula to be correlated with the function of the retina. The results of this test have been used to help patients whose diagnosis is challenging or who have questions about the rate of progression of their condition from one year to another. This study is often helpful for patients with early and mid stages of macular degeneration