Before getting started, read our Retina 101 page.
What is diabetic retinopathy?
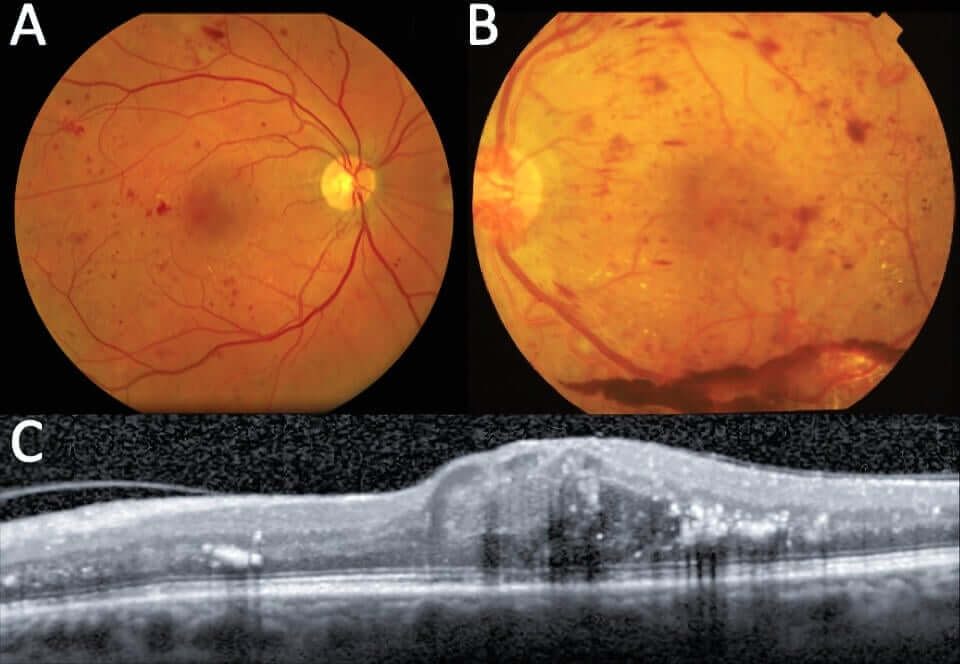
Diabetes is a very common medical condition characterized by a deficiency of or resistance to insulin, and associated with elevated blood sugar (hyperglycemia). Chronic hyperglycemia damages blood vessels, including those in the eye. If you consider the blood vessels of the eye like a tree, diabetes begins with damage to the smallest vessels – the twigs of the tree. Damaged vessels become weak and can leak fluid as well as form small blisters along the walls. These blisters can burst, leading to retinal hemorrhages.
Progressive vascular damage can lead to loss of blood supply to large areas of the retina (ischemia), leading to production of toxic chemicals that further promote vascular irregularities, leakage, and, eventually, growth of dangerous new blood vessels. Vascular leakage in the macula leads to retinal swelling and blurred vision. New blood vessels are very weak and can bleed easily and may grow into the vitreous like vines growing on a scaffold, eventually detaching the retina from the back wall of the eye.
Click here to learn more about our clinical trials.
Symptoms of Diabetic Retinopathy
Symptoms of diabetic retinopathy can vary significantly. Patients with mild diabetic retinopathy are usually asymptomatic. Diabetic macular edema usually causes central blurring of the vision.
Patients with significant hemorrhage or retinal detachment typically note a loss of vision with new haze and floaters. Severe, untreated eyes can become very sick and may become completely and irreversibly blind. This is typically avoidable with treatment.
Additional Findings
There is a fairly broad spectrum of findings in diabetic retinopathy, including microaneurysms, small retinal hemorrhages, irregular vascular contour, new blood vessel growth off the surface of the optic nerve and/or retina, bleeding in front of the retina and/or into the vitreous, and retinal detachment.
The severity of these findings depends on the duration and control of diabetes, blood pressure control, and smoking status. Leakage from damaged blood vessels in the macula can lead to swelling and reduced vision.
Diabetic Retinopathy Treatment
The most important “treatment” for diabetic retinopathy is prevention with excellent blood sugar and blood pressure control, healthy lifestyle, and avoidance of smoking. Patients should target having a hemoglobin A1c under 7.0.
Most eyes with mild to moderate diabetic retinopathy do not require any treatment. Eyes are observed at regular intervals or worsening of retinopathy and development of new blood vessels or diabetic macular edema.
Patients with severe diabetic retinopathy and/or diabetic macular edema may be treated with medications injected into the eye that reverse vessel abnormalities, including aneurysms, hemorrhages, leakage, and new vessel growth.
Outcomes
Patients with diabetic retinopathy and diabetic macular edema can do very well if caught early and can maintain excellent vision for the rest of their lives. Most patients with vision loss due to macular edema have significant improvement once treatment is started.
Patients who need surgery for severe bleeding or retinal detachment can also do well, but the risk of permanent vision loss increases, and may be profound.

