Before getting started, read our Retina 101 page.
What are retinal tears and detachments?
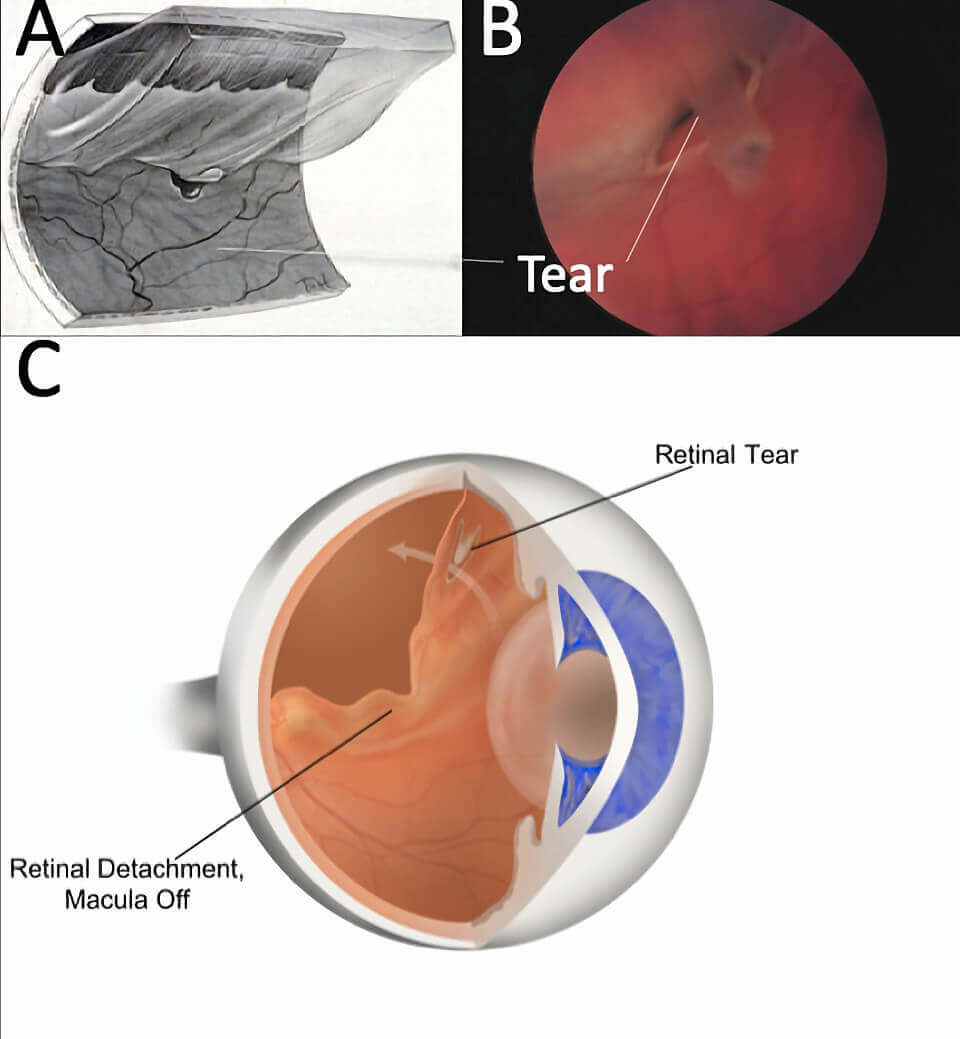
Think of the process of vitreous detachment as peeling tape (ie. the edge of the vitreous) off very thin wallpaper (ie. the retina). Most often the adhesion between the vitreous and retina is light, similar to scotch tape, but near the front of the eye and periphery of the retina the adhesion is significantly stronger, more similar to duct tape.
Forceful separations can tear the retina and liquid from the vitreous can get under the tear, leading to separation of the retina from the underlying tissue like wallpaper peeling off a wall, called a retinal detachment.
Symptoms of Retinal Tears and Detachments
The most common symptom of a retinal tear is prominent, crescent-like flashes of light in the peripheral vision of one eye. Patients may also notice a sudden onset of new floaters – often described as a shower of black dots. These symtoms are often prominent, but may be subtle, and occasionally we see retinal tears in patients with no symptoms. On the other hand, some retinal tears are associated with significant bleeding into the eye, with associated blurred vision.
A retinal detachment is associated with a dark curtain in the vision, starting from the periphery. Central vision may be good unless the macula is involved.
Additional Findings
Retinal tears are commonly visible in the peripheral retina as a “U” shaped flap of tissue. Eyes typically have a PVD, and may have blood and/or pigment dust as a result of the tear visible in the vitreous. Some tears have separated from the rest of the retina, called “operculated” tears. Eyes with a retinal detachment have a variable amount of fluid beneath and surrounding the tear.
Retinal Tears and Detachments Treatment
Retinal tears in and of themselves are fairly benign. It is the risk of progression to a retinal detachment, where liquid vitreous passes through the tear, that must be prevented.
To prevent this, the tear simply needs to be barricaded where the tissue around the tear is secured to the underlying wall of the eye. This is commonly done with laser, but cryotherapy may be used in some situations, particularly if there is blood obscuring the view. Either of these options will form a scar around the tear to minimize the risk of it progressing to a detachment, but do not treat the tear itself, or any of the symptoms of the tear.
Very small retinal detachments may be able to be barricaded with laser, but most will require surgical repair. There are three main options for this that will vary depending on the clinical situation and include pneumatic retinopexy, vitrectomy, and scleral buckling.
Outcomes
Most patients treated for a retinal tear do very well. Floaters and flashing lights will eventually resolve over time, taking weeks to months. We are also very successful at repairing retinal detachments with over a 95% success rate. If the macula was involved in the detachment there will be a variable amount of vision loss, depending on the duration of the detachment.

